CHOP and Keystone First Contract Negotiations Continue
The Children’s Hospital of Philadelphia (CHOP) is a participating provider with Keystone First and AmeriHealth Caritas PA, two of the biggest Medicaid managed care organizations (MCOs) in Pennsylvania. The contract between CHOP and Keystone/AmeriHealth is set to end on July 1, 2024, unless a new agreement is reached before that date. If the contract ends, CHOP hospitals, all CHOP doctors, and CHOP Home Care will no longer be in-network for members in Keystone First or AmeriHealth.
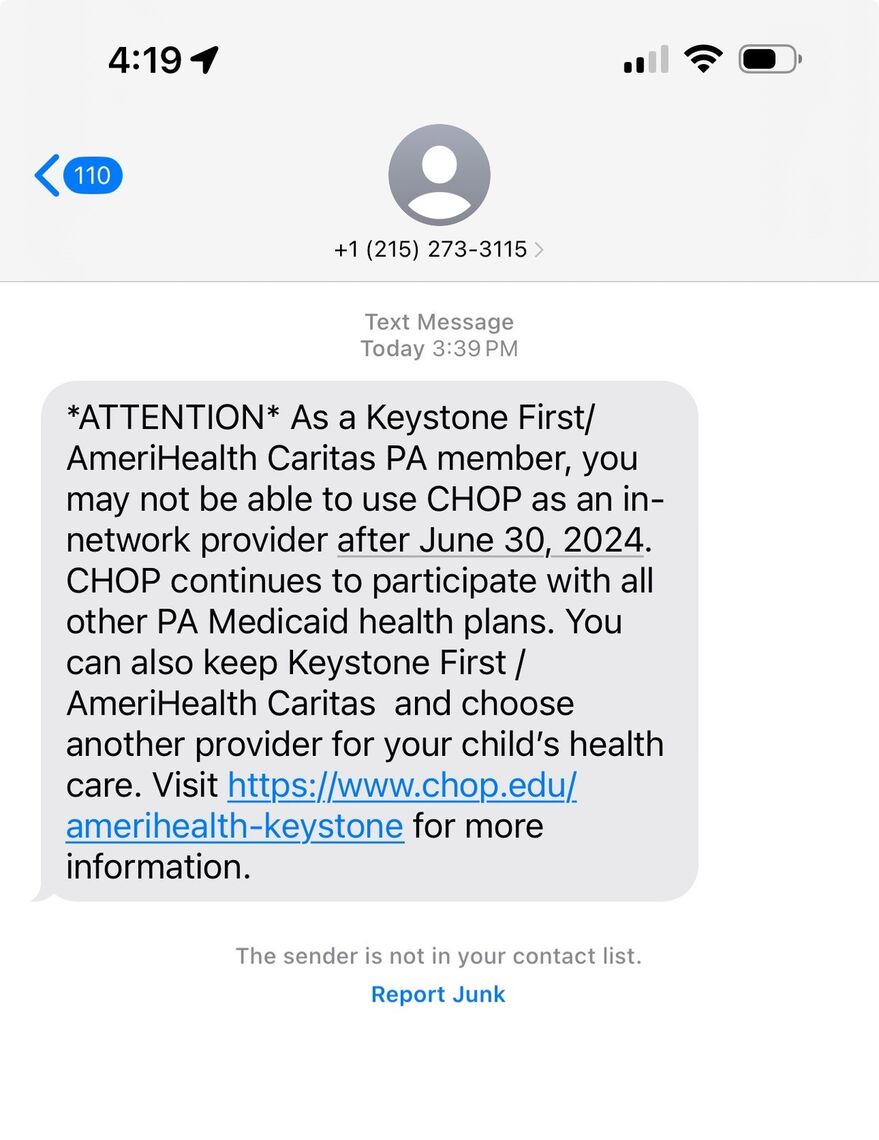
Keystone/AmeriHealth must tell the state at least 60 days in advance of any contract breaks, meaning they must notify the state by May 1st if the contract is going to end. Despite this timeline, in late March, CHOP elected to notify their Keystone/AmeriHealth patients of the potential contract break. CHOP sent text messages and emails to approximately 150,000 patients advising them of an upcoming end to their contract with Keystone/AmeriHealth if negotiations are unsuccessful. A copy of the text sent by CHOP, which directed families to this CHOP FAQ website, is below:
What can I do if the contract ends?
If CHOP and Keystone/AmeriHealth are unable to reach a new agreement by June 30th, families will have two choices for their child's ongoing care and coverage: pick a new MCO and stay with existing CHOP doctors; or stay with Keystone/AmeriHealth and pick new doctors. Each choice is explained below, along with information about the continuity of care rules, which can allow children to keep seeing their CHOP doctors and other providers after July 1 by making a special request to Keystone/AmeriHealth.
1. Pick a new MCO and stay with existing CHOP doctors
The good news is that CHOP is in network with all other MCOs in Southeast Pennsylvania, including Health Partners, UPMC for You, Geisinger, United, and Highmark Wholecare. Of course, the decision to change your child’s MCO is not one that should be made lightly. If your child sees many other specialists, gets care from a home health agency, receives outpatient therapies, or gets supplies and equipment from a Durable Medical Equipment (DME) supplier, try to try to pick an MCO that has as many of those providers in network as possible, including your child’s CHOP providers.
For the new coverage to be effective July 1st, families must choose a new MCO by Thursday, June 13th! Changes made June 14th or later will not be effective until August 1st at the earliest. Our self-help guide, Tips for Choosing a Health Plan, has step by step instructions for how to switch MCOs and what to consider when doing so.
To compare available MCOs, search MCO provider networks, and enroll in a new MCO:
- Visit the PA Enrollment Services website at www.EnrollNow.net;
- Use the PA Enrollment Services app (download from Apple Store or Google Play); or
- Call PA Enrollment Services at 1-800-440-3989 (TTY: 1-800-618-4225).
2. Stay with Keystone/AmeriHealth and pick new doctors
Just like the decision to pick a new MCO is one that should not be made lightly, picking new doctors and other providers is also not easy and should be done with careful consideration and planning. Finding all new doctors and other healthcare providers may not even be possible for some children, especially those who see several specialists, are being treated for a rare condition or disorder, or who have long, established relationships with their CHOP doctors.
To find other providers in the Keystone/AmeriHealth network(s), visit the Find a Provider section of EnrollNow.net, or call AmeriHealth Member Services at 1-888-991-7200 or Keystone First Member Services at 1-800-521-6860 to ask for a list of other in-network doctors and other providers.
Continuity of Care
Children who stay enrolled in Keystone/AmeriHealth after July 1 can keep seeing their CHOP doctors for up to 60 days by requesting “continued coverage” from Keystone or AmeriHealth. The continued coverage or “continuity of care” rules allow members to keep seeing their out-of-network doctors and other healthcare providers for a certain period following changing MCOs or their provider leaving their MCO’s network. This applies both to services that receive prior authorization and to ongoing courses of treatment that do not need prior authorization. Continuity of care rights are defined in the state’s contract with the Medicaid MCOs, known as the HealthChoices Agreement. A member whose request for continued coverage is denied has the right to appeal that decision. Additionally,
Impacted families can request help coordinating their child’s care transitions by contacting the Keystone First Special Needs Unit at 1-800-573-4100 (TTY: 711) or the AmeriHealth Caritas Special Needs Unit at 1-800-684-5503 (TTY: 711).
Families with questions about CHOP’s contract with Keystone/AmeriHealth should visit the CHOP website for more information: AmeriHealth Caritas PA and Keystone First Contract Termination: Answering a Family's Questions | Children's Hospital of Philadelphia (chop.edu), or call AmeriHealth Member Services at 1-888-991-7200 or Keystone First Member Services at 1-800-521-6860. We will continue monitoring the CHOP/Keystone contract situation and will provide updates as we learn them.
