In the early 1980s, several attorneys from the Delaware County Legal Assistance Association (DCLAA) and the Bucks County Legal Aid Society (BCLAS)—Ann Torregrossa, Michael Campbell, Dana Breslin, David Gates, and Nancy Schuster—began collaborating on cases to assure that Medicaid services were both accessible and of high quality for Pennsylvania’s poor.
One of PHLP’s first cases was Simpson v. Schweiker. In 1981, if you were low-income, pregnant, and living in Pennsylvania the medical standard for prenatal care simply did not apply to you. Specifically, Pennsylvania’s Medicaid program refused to pay for ultrasounds, substituting x-rays as a “compensable alternative” for monitoring the progress of a pregnancy. PHLP sued the state on behalf of clients needing up-to-date, quality health care. The settlement agreement made more than 800 modern medical procedures available to Medicaid recipients. This was the launching point of PHLP; to tear down the barriers to healthcare that stand in the way of those who need it most.
During PHLP’s early years, Pennsylvania became a national testing ground for prepaid managed care for the poor. In 1986, the federal government allowed Pennsylvania to contract with the private sector to create HealthPASS, a managed care program available to Medicaid recipients in south and west Philadelphia. The assigned contractor, Healthcare Management Alternatives (HMA), received a fixed, prepaid, monthly payment for approximately 76,000 Medicaid recipients. PHLP was not supportive of the new arrangement but worked to ensure clients’ interests were represented in program design and throughout implementation.
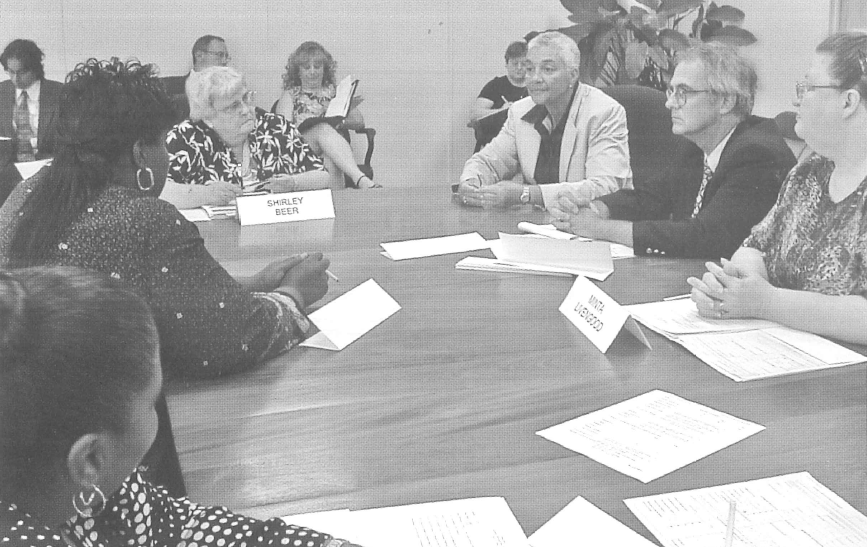
PHLP also became legal counsel to several client groups, most notably the Consumer Subcommittee of Pennsylvania’s Medical Assistance Advisory Committee (MAAC), headed by Louise Brookins. As legal counsel to the Consumer Subcommittee, PHLP briefed consumers on health issues, providing technical assistance, and identifying and interpreting legal issues. The Subcommittee (still in existence) is one of the most active Medicaid consumer advisory committees in the country.