Revamped Annual Assessment Process to Determine Participants’ Continued Eligibility for CHC Waiver
Earlier this year, the Community HealthChoices (CHC) program implemented a new, streamlined process to reassess the clinical eligibility of enrollees in the CHC Waiver. Since a person’s clinical waiver eligibility must be reviewed annually, CHC plans conduct these evaluations at least once a year to confirm that those enrolled in the Waiver still meet the requirements. A person remains clinically eligible for the CHC Waiver if they require the level of care typically provided in a nursing facility. These individuals are considered "nursing facility clinically eligible" (NFCE).
CHC plans began performing these annual reassessments for the first time in mid-2023. At the start of this process, thousands of Pennsylvanians were removed from the CHC Waiver despite appearing to still meet the eligibility criteria. Acknowledging potential issues in the reassessment process that led to individuals mistakenly losing their coverage, the Department of Human Services adjusted the process to improve how the reassessments address the needs and eligibility of CHC waiver participants.
What's Changed?
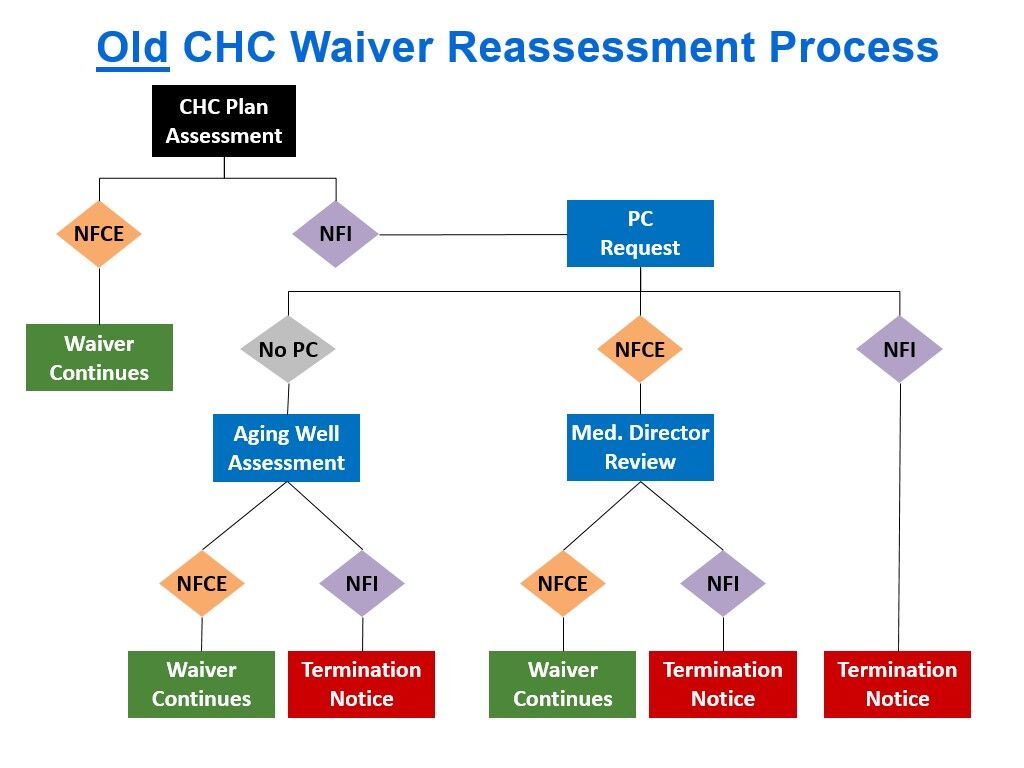
For an overview of the process as it existed back in 2023, please see our prior post here.
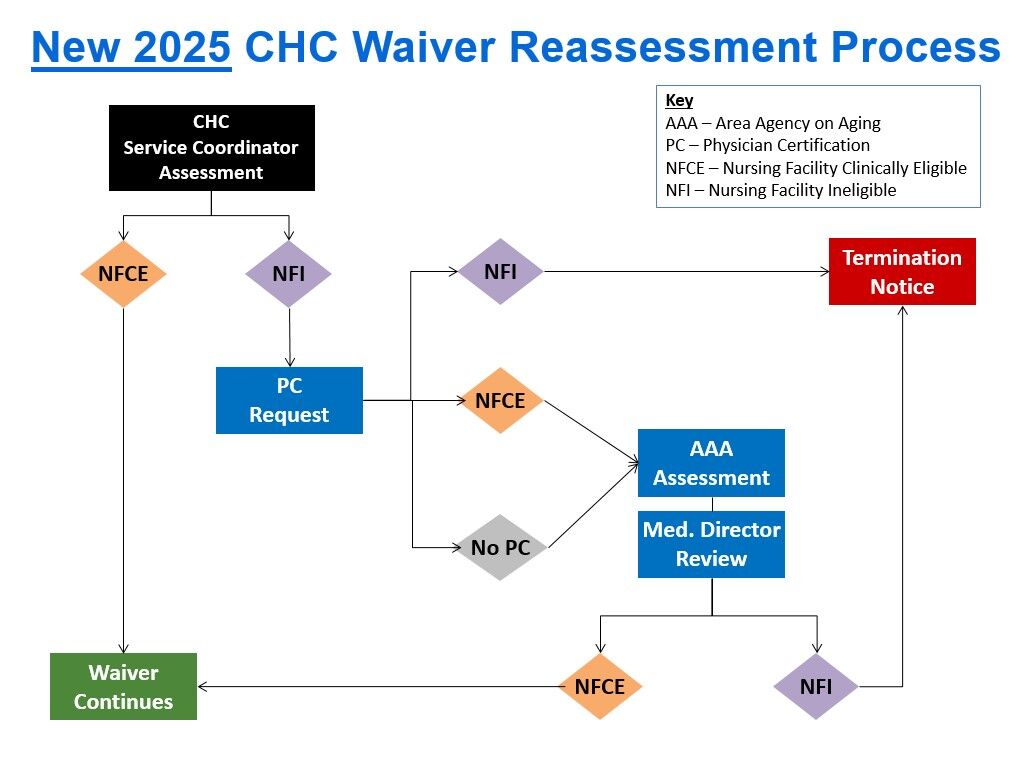
The new process still uses as a starting point the results of all prior comprehensive needs assessments conducted by a CHC participant’s service coordinator. This means that both the CHC plan’s annual reassessment and any assessments conducted in between are not only used to determine what services a person needs, but also whether the person remains eligible for the CHC waiver. Most people are found to remain eligible after their reassessment. However, if the reassessment indicates a person is no longer eligible for the waiver, the CHC plan contacts that person’s doctor to have them complete a “Physician Certification Form” stating whether the person meets the level of care (NFCE) for the CHC waiver. From this point, the reassessment process has changed depending on whether and how the doctor completes that form:
- If the doctor checks the box on the physician certification form stating the person is “nursing facility ineligible” (NFI) -- in other words indicating the participant does not meet the waiver level of care requirement -- the Department of Human Services’ Independent Assessment Entity (IAE) sends a notice to the participant informing them they will be terminated from the CHC waiver and explaining their appeal rights.
- If the person’s doctor does not return the physician certification form or if the doctor checks the box indicating the person is nursing facility clinically eligible, the IAE will ask the local Area Agency on Aging (AAA) to contact the person to schedule a new functional eligibility assessment. This is the same assessment that is done when someone first applies for the CHC waiver and is not as lengthy as the needs assessments that service coordinators conduct.
NOTE: CHC participants should cooperate with the AAA to complete this assessment or risk receiving a notice terminating them from the waiver. Different AAAs may have different practices for reaching out to schedule the assessment. In PHLP’s experience, the AAA will call the participant first and, if they can’t reach them, follow up with a letter. The letters PHLP has seen are confusing as they imply that the person is a new applicant for the CHC waiver, rather than someone who is currently on the waiver who needs to be reevaluated so they can continue to receive the waiver.
- After the AAA completes its assessment, OLTL’s medical director team reviews both the AAA and service coordinator assessments, the physician certification (if any), other assessments from the past 12 months, service coordinator notes, and the most recent service plan. After reviewing these materials, the OLTL medical director makes a final decision as to whether the person continues to be clinically eligible for the CHC waiver. If they are not, they will receive a waiver termination notice they can appeal. If they are still eligible, it is not clear how the participant is informed of this; at least one PHLP client reported being told by the AAA by phone.
Although there is no data yet available to compare how waiver participants are faring under the revamped process, PHLP has noticed a dramatic decrease in calls to our Helpline from people losing the CHC waiver following their annual reassessment. The calls we have received generally involve people whose doctors said they were ineligible or who have questions about why the AAA is contacting them for an assessment.
Reassessment Tips
Here are a few tips to ensure that any assessment by a service coordinator or the AAA is accurate:
- If possible, have a trusted family member or caregiver who understands the CHC participant’s needs present at any assessment. These individuals may be able to help participants express their needs and any challenges they have. This is especially important for people who have a brain injury or other cognitive impairment that might limit insight into their condition. Some of the questions on the assessments used to determine ongoing eligibility pertain to cognition so ensuring answers to those questions are accurate is critical. In PHLP’s experience, assessments by service coordinators often miss problems with cognition which has led to inappropriate waiver terminations.
- Do not understate needs or any limitations or challenges. It can be embarrassing to share with strangers intimate details about the help someone needs and why. But being honest and clear about needs and challenges is critical to ensuring an accurate assessment.
Looking Ahead
There are questions remaining about how people with developmental disabilities – i.e., those disabilities with onsets before age 22—will fare under the new process. Those determined NFI as a result of a reassessment should be evaluated for the OBRA waiver instead. The OBRA waiver serves people with developmental disabilities and has a different (lower) clinical eligibility requirement than the NFCE standard used for CHC. It is not clear how or whether such individuals are assessed for the OBRA waiver before they are removed from the CHC waiver following a reassessment.
Appealing Waiver Terminations
If you receive a waiver termination notice following your annual reassessment, you can and should file an appeal to challenge that decision. Appeals must be filed in writing (email works!) Be sure to file the appeal within 15 days of the termination notice to keep your waiver coverage & services active while the appeal is pending.
Once you file the appeal, contact Aging Well at 1-888-204-0946 or info@agingwellpa.org to ask for a copy of all materials that were used or reviewed as part of your reassessment. You have a legal right to this information and it must include everything that the OLTL Medical Director reviewed.
If you need legal help because you are being terminated from the CHC waiver or experiencing a gap in coverage or care following a timely appeal, contact your local legal aid office or PHLP’s Helpline at 1-800-274-3258.
